Vulvar vs Vaginal vs Perineal Warts: How Location Affects Treatment
How advanced non-surgical laser technology treats vulvar, vaginal, and perineal lesions
12/22/20253 min read


Genital warts, caused by certain strains of the human papillomavirus (HPV), are common—but their location plays a critical role in how they are safely and effectively treated. Warts that appear on the vulva, inside the vagina, or along the perineum each involve different tissue types, sensitivity levels, and healing dynamics.
For patients seeking non-surgical treatment options, modern laser technology offers a precise, tissue-sparing alternative to traditional excision. At Spectra Athenova, we support clinicians with advanced energy-based platforms—such as the Fotona TimeWalker® II IntimaLaser™ system equipped with the MicroPilot M100 handpiece—designed for controlled treatment of vulvar and cervical lesions while prioritizing comfort, healing, and aesthetic outcomes.


Here’s how wart location influences laser treatment strategy.
Understanding the Three Key Areas
1. Vulvar Warts (External Genital Skin)
The vulva includes the labia majora, labia minora, and clitoral hood—areas composed of thicker external skin.
What they look like:
Flesh-colored, pink, or grey growths
Flat, raised, or cauliflower-like in appearance
Often visible and easier to identify early


Laser treatment considerations:
Because vulvar skin is more resilient, non-surgical laser therapy can be applied with high precision to target wart tissue while preserving surrounding healthy skin. Platforms such as Fotona TimeWalker® II with the MicroPilot M100 allow clinicians to:
Deliver controlled energy to superficial lesions
Minimize bleeding and tissue trauma
Reduce scarring and support favorable cosmetic outcomes
Promote faster recovery compared to surgical methods
Key advantage:
Visibility enables early diagnosis and straightforward laser targeting.
2. Vaginal and Cervical Warts (Internal Mucosal Tissue)
Warts affecting the vaginal canal or cervix develop on delicate mucosal tissue that requires a refined treatment approach.
What they feel like:
Often asymptomatic
Sometimes associated with irritation, discharge, or spotting
Typically identified during gynecologic examination
Laser treatment considerations:
Internal mucosa demands exceptional precision and low-trauma techniques. The MicroPilot M100 handpiece, designed specifically for gynecologic applications, supports clinicians in treating vaginal and cervical lesions by enabling:
Accurate energy delivery without incisions or sutures
Preservation of healthy mucosal tissue
Reduced risk of scarring or excessive inflammation
Improved patient comfort during and after treatment
Self-applied therapies are not appropriate for internal lesions—professional, controlled laser treatment is essential in these anatomically sensitive areas.
Key challenge:
Limited access and fragile tissue make precise targeting and energy modulation critical.
3. Perineal Warts (Between the Vagina and Anus)
The perineum is subject to friction, moisture, and movement, which can complicate healing.
What makes this area unique:
Continuous mechanical stress from walking, sitting, and clothing
Higher risk of irritation if tissue trauma is excessive
Laser treatment considerations:
Non-surgical laser therapy allows clinicians to:
Target lesions without cutting or suturing
Minimize collateral tissue damage
Support faster epithelial recovery
Reduce the likelihood of infection or prolonged discomfort
Although the MicroPilot M100 is specifically optimized for vulvar and cervical applications, advanced laser systems across the TimeWalker® II platform can be adapted for perineal treatments with appropriate technique and parameter selection.
Key focus:
Effective wart removal with minimal tissue disruption to support healing in a high-movement area.
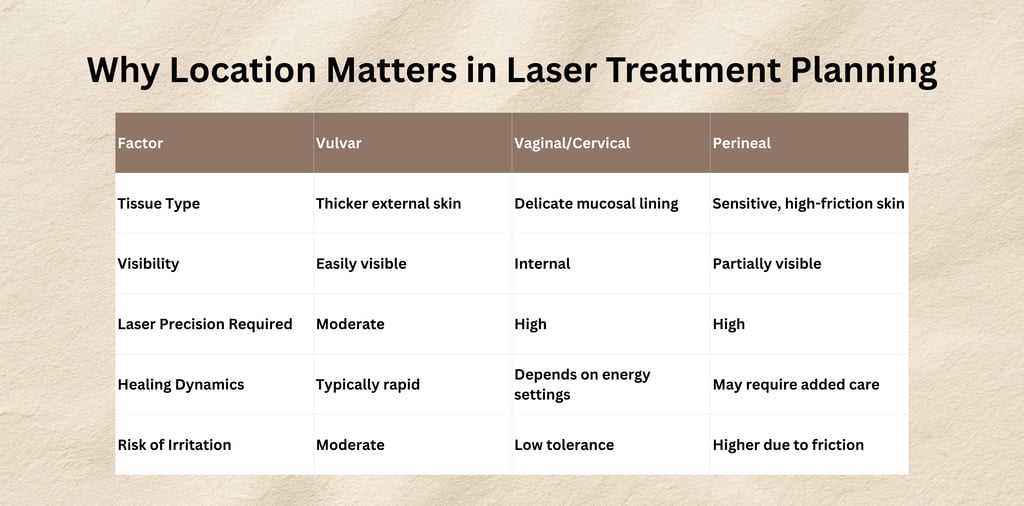
Laser parameters—such as wavelength, pulse duration, and energy density—must be carefully adjusted based on anatomical location and tissue response. Specialized tools like the MicroPilot M100 are engineered to support accurate treatment of sensitive vulvar and cervical tissue while reducing unnecessary thermal spread.
The Advantages of Non-Surgical Laser Technology
Modern gynecologic laser platforms offer:
Targeted tissue interaction with minimal impact on surrounding structures
Bloodless or low-bleeding procedures
Reduced discomfort and downtime compared with surgical excision
Improved cosmetic and functional outcomes
The ability to treat delicate anatomical regions with precision and control
At Spectra Athenova, advanced systems such as Fotona TimeWalker® II IntimaLaser™ enable clinicians to tailor therapy based on lesion size, depth, recurrence history, and anatomical location, supporting individualized, patient-centered care.
When to Seek Professional Evaluation
Patients should consult a qualified healthcare provider if they notice:
New or changing growths in the genital area
Persistent irritation, itching, or bleeding
Recurrence after previous treatment
Early evaluation often allows for less invasive laser-based management and reduces the risk of progression or spread.
A Precision-Driven Approach to Intimate Health
Genital warts are treatable, but their location determines the safest and most effective treatment pathway. Vulvar, vaginal/cervical, and perineal lesions each require tailored laser settings, technique, and aftercare.
With technologies such as the Fotona TimeWalker® II IntimaLaser™ platform, non-surgical laser therapy offers a modern, tissue-preserving approach—designed for precision in even the most sensitive anatomical areas.
Spectra Athenova is a specialized healthcare solutions division by Spectra Medical, dedicated to advancing science-led innovations in aesthetics, dermatology, and anti-aging medicine. With a strong focus on clinical intelligence, education, and evidence-based technologies, Spectra Athenova partners with healthcare professionals to elevate patient outcomes and shape the future of aesthetic medicine.
Spectra Athenova
Miscellaneous
